Platelet Aggregation Studies
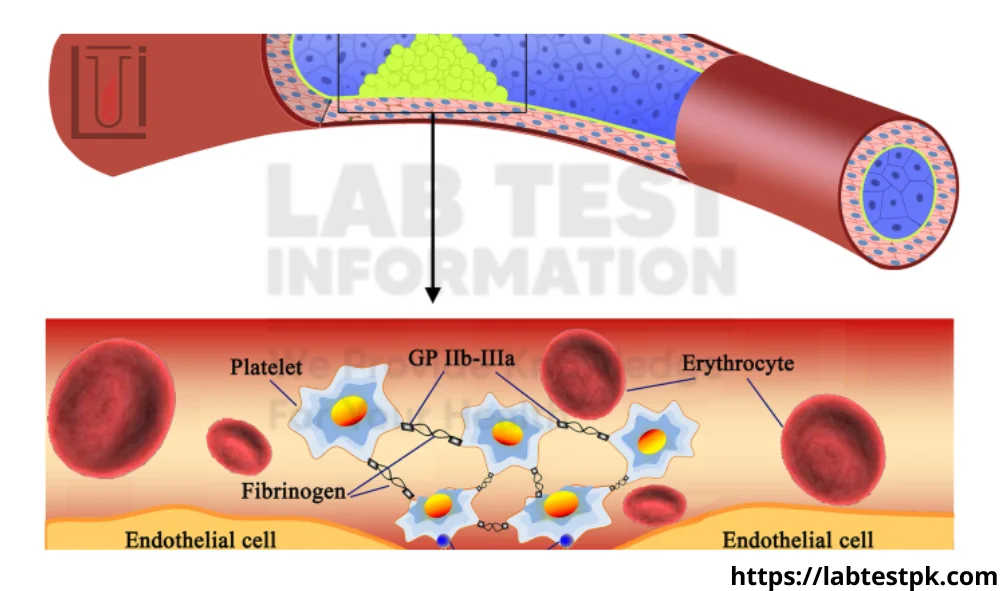
Platelet Aggregation Studies is a type of laboratory test that assesses how well platelets in the blood stick together. Platelets are small cell fragments in the blood that play a crucial role in blood clotting and wound healing. Platelet aggregation is a normal and necessary process to prevent excessive bleeding, but abnormal platelet aggregation can lead to inappropriate blood clot formation, which may contribute to conditions such as heart attacks and strokes.
The platelet aggregation studies involve exposing a blood sample to various substances that promote platelet activation and aggregation. The response of the platelets to these substances is then measured to evaluate their function. Some common substances used in platelet aggregation studies include:
- ADP (adenosine diphosphate): ADP is released by damaged cells and helps to activate platelets. Testing platelet aggregation in response to ADP provides information about the platelet response to this common activator.
- Collagen: Collagen is a protein found in the walls of blood vessels. Platelets adhere to collagen when exposed to it, and this interaction is important in the formation of blood clots.
- Epinephrine: Epinephrine, also known as adrenaline, is a hormone that can activate platelets and enhance their aggregating response.
- Arachidonic acid: This substance is involved in the production of thromboxane, a compound that promotes platelet aggregation.
- Ristocetin: Ristocetin is an antibiotic that induces platelet aggregation by causing it to bind to von Willebrand factor, a protein involved in blood clotting.
Platelet aggregation studies are used in the diagnosis and management of various conditions, including bleeding disorders and clotting disorders. Abnormal platelet aggregation can be indicative of platelet function disorders, which can be congenital or acquired. Additionally, these studies are relevant in monitoring the effects of antiplatelet medications, such as aspirin or clopidogrel, which are commonly prescribed to reduce the risk of clot formation in conditions like heart disease.
Why is the test performed?
Here are some specific reasons why the platelet aggregation test is performed:
- Diagnosis of Platelet Function Disorders: Platelet aggregation studies help diagnose conditions where platelets do not function properly. Some individuals may have congenital (inherited) platelet function disorders, such as Glanzmann thrombasthenia or Bernard-Soulier syndrome, which affect the ability of platelets to aggregate and form clots.
- Evaluation of Bleeding Disorders: Abnormal platelet function can contribute to bleeding disorders. Platelet aggregation tests can be part of a battery of tests used to investigate the cause of abnormal bleeding, such as easy bruising, prolonged bleeding from minor injuries, or excessive bleeding during surgery.
- Monitoring Antiplatelet Medication: Antiplatelet medications, such as aspirin or clopidogrel, are commonly prescribed to prevent blood clot formation in conditions like coronary artery disease. Platelet aggregation studies may be used to monitor the effectiveness of these medications by assessing the degree of platelet inhibition.
- Assessment of Thrombocytopathy: Thrombocytopathy refers to disorders where platelets do not function properly even though their numbers are normal. Platelet aggregation tests help identify and characterize these disorders.
- Investigation of Platelet Disorders in Pregnancy: Some pregnant women may develop conditions like gestational thrombocytopenia, where platelet function is impaired. Platelet aggregation studies can be part of the evaluation for these conditions.
- Research and Clinical Studies: Platelet aggregation studies are also used in research settings to better understand the mechanisms of platelet function and to explore potential treatments for platelet-related disorders.
What are the symptoms of a low platelet count?
Common symptoms of a low platelet count include:
- Petechiae: These are small, pinpoint-sized red or purple spots on the skin that result from tiny blood vessels (capillaries) leaking blood. They may look like a rash and are particularly common on the lower legs.
- Purpura: Purpura refers to larger areas of bleeding under the skin, causing purple or red discoloration. Like petechiae, purpura occurs due to bleeding from small blood vessels.
- Ecchymosis: This term describes larger bruises that result from bleeding beneath the skin. People with low platelet counts may bruise easily, and the bruises may be larger than expected from minor injuries.
- Nosebleeds: Spontaneous or prolonged nosebleeds can occur when the blood vessels in the nose are not able to clot effectively.
- Gum Bleeding: Bleeding from the gums, especially after brushing the teeth or flossing, may occur in individuals with low platelet counts.
- Blood in Urine or Stool: Thrombocytopenia can lead to bleeding in the gastrointestinal tract, which may result in blood appearing in the urine or stool.
- Excessive Menstrual Bleeding: Women with low platelet counts may experience heavier or prolonged menstrual bleeding.
- Excessive Bleeding After Injury or Surgery: Even minor injuries or surgical procedures can result in prolonged bleeding or difficulty stopping bleeding in individuals with low platelet counts.
It’s important to note that thrombocytopenia can have various causes, including underlying medical conditions, medications, infections, autoimmune disorders, and bone marrow disorders.
What are the causes of a low platelet count?
A low platelet count, or thrombocytopenia, can have various causes, and it may be due to decreased production, increased destruction, or sequestration of platelets. Some common causes include:
- Bone Marrow Disorders:
- Aplastic Anemia: A condition where the bone marrow doesn’t produce enough blood cells, including platelets.
- Myelodysplastic Syndromes (MDS): Disorders characterized by abnormal development and function of blood cells in the bone marrow.
- Increased Platelet Destruction:
- Immune Thrombocytopenic Purpura (ITP): An autoimmune disorder where the immune system mistakenly attacks and destroys platelets.
- Drug-Induced Thrombocytopenia: Some medications can cause the immune system to destroy platelets. Examples include heparin, certain antibiotics, and some anti-seizure medications.
- Viral Infections:
- HIV/AIDS: The human immunodeficiency virus (HIV) can affect the bone marrow and lead to thrombocytopenia.
- Hepatitis C: Some individuals with hepatitis C may experience decreased platelet counts.
- Certain Cancers:
- Leukemia: Cancer of the blood and bone marrow can affect platelet production.
- Lymphoma: Certain types of lymphoma may lead to decreased platelet counts.
- Chemotherapy and Radiation Therapy:
- Cancer treatments can suppress bone marrow function, affecting platelet production.
- Inherited Conditions:
- Congenital Amegakaryocytic Thrombocytopenia: A rare inherited disorder affecting platelet production.
- Wiskott-Aldrich Syndrome: An X-linked genetic disorder that can cause low platelet counts.
- Hypersplenism:
- An enlarged spleen (splenomegaly) may sequester and remove platelets from circulation.
- Certain Autoimmune Disorders:
- Systemic Lupus Erythematosus (SLE): An autoimmune disease that can affect multiple organs, including the blood.
- Rheumatoid Arthritis: Some individuals with rheumatoid arthritis may develop thrombocytopenia.
- Pregnancy-Related Causes:
- Gestational Thrombocytopenia: A condition where platelet counts decrease during pregnancy.
- Heparin-Induced Thrombocytopenia (HIT):
- An immune reaction to heparin, an anticoagulant medication, leads to a decrease in platelet counts.

[…] that develop inside the mouth. They can appear on the tongue, inside of the cheeks, or on the gums. Canker sores are usually round or oval-shaped with a white or yellow center and a red border. They […]
[…] Autoimmune disorders […]