Food Allergy Panel
Food Allergy Panel, A food allergy panel, also known as a food allergy test, is a medical test designed to identify specific food allergens that may be causing allergic reactions in an individual. Food allergies occur when the immune system mistakenly identifies certain proteins found in certain foods as harmful invaders, leading to an immune response that can cause a range of symptoms, from mild to severe.
There are different types of food allergy tests, and each has its advantages and limitations:
- Skin Prick Test: This is a standard method where a small number of allergenic extracts from various foods are applied to the skin, usually on the forearm or back. The skin is then lightly pricked or scratched to introduce the allergens under the skin’s surface. A small raised bump or hive may develop at the test site within 15-20 minutes if a person is allergic to a particular food.
- Blood Test (Specific IgE Test): This test measures the levels of specific antibodies called immunoglobulin E (IgE) in the blood that are produced in response to allergens. The results are reported as numerical values for various allergens. Common blood tests include the ImmunoCAP test and the RAST test.
- Patch Test: This is used less frequently for food allergies and is more commonly used for testing contact allergies (allergies to substances that come into direct contact with the skin). Small amounts of food extracts are applied to patches that are placed on the skin for a certain period. Reactions are evaluated after a couple of days.
- Elimination Diet: While not a direct test, this method involves removing specific foods from the diet and observing whether allergic symptoms improve. This is often followed by gradually reintroducing the eliminated foods to pinpoint the specific allergens.
- Oral Food Challenge: This is considered the gold standard for diagnosing food allergies. Under medical supervision, a person is given gradually increasing amounts of the suspected allergen to consume. Any reaction is closely monitored and managed.
It’s important to note that the interpretation of food allergy tests requires a trained medical professional. False positive or false negative results can occur, and the results should be considered alongside a person’s medical history and clinical symptoms. Also, the presence of positive test results doesn’t always indicate a clinical allergy – some people may test positive but not experience allergic reactions when consuming the foods.
If you suspect you have a food allergy, it’s recommended to consult with a healthcare provider, preferably an allergist or immunologist, who can guide you through the appropriate testing and interpretation of results. They can also help develop an appropriate management plan based on your situation.
Types of Food Allergy:
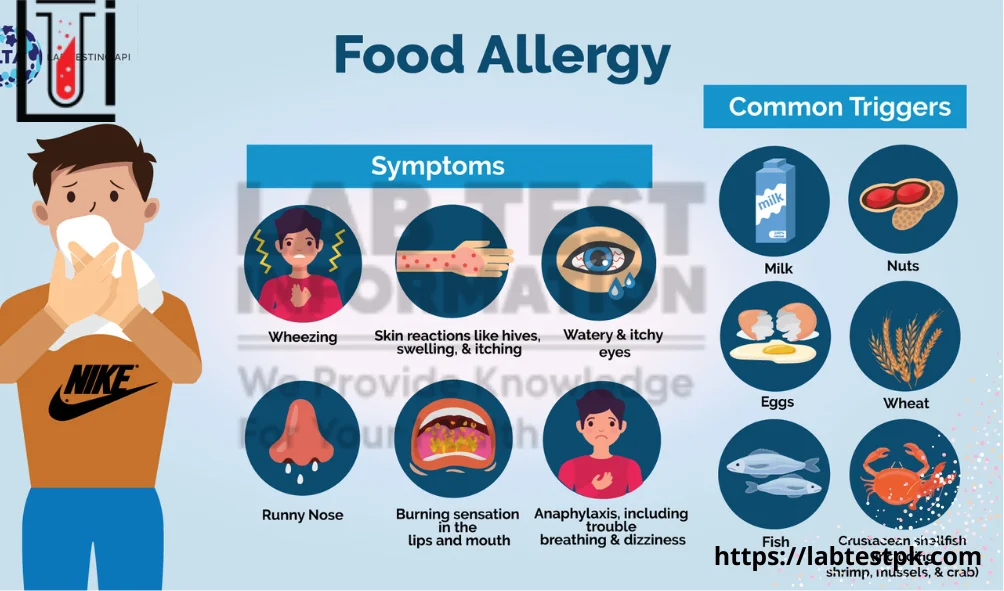
Food allergies are immune system reactions that occur when the body mistakenly identifies certain proteins in food as harmful invaders. These reactions can range from mild to severe and can occur within minutes to a few hours after consuming the allergenic food. Here are some common types of food allergies:
- Milk Allergy: This is an allergic reaction to proteins found in cow’s milk and dairy products. Symptoms can include hives, digestive issues, and in severe cases, anaphylaxis.
- Egg Allergy: Egg allergies typically involve a reaction to proteins found in egg whites or yolks. Symptoms can range from skin reactions to gastrointestinal discomfort.
- Peanut Allergy: Peanut allergies can cause severe reactions, including anaphylaxis. Even trace amounts of peanuts can trigger symptoms in some individuals.
- Tree Nut Allergy: This includes allergies to various tree nuts such as almonds, walnuts, cashews, and pistachios. These allergies can also cause severe reactions.
- Soy Allergy: Some people may be allergic to soy proteins, commonly found in products like soy milk, tofu, and soy sauce.
- Wheat Allergy: This is an allergy to proteins found in wheat, including gluten. It can cause symptoms ranging from mild skin reactions to more serious digestive issues.
- Fish Allergy: Allergic reactions to fish proteins can be severe and may lead to anaphylaxis. It’s important to note that some individuals are allergic to specific types of fish while being able to tolerate others.
- Shellfish Allergy: This includes allergies to both crustaceans (such as shrimp, crab, and lobster) and mollusks (such as clams, mussels, and oysters). Shellfish allergies can also cause severe reactions.
- Sesame Allergy: Sesame allergies have gained more attention in recent years. Sesame seeds and sesame oil are common ingredients in various foods.
- Mustard Allergy: Mustard allergy can cause symptoms ranging from mild to severe. It’s commonly found in prepared foods, sauces, and condiments.
- Sulfite Sensitivity: While not a true allergy, some individuals may be sensitive to sulfites, which are preservatives commonly used in certain foods and drinks.
- Cross-Reactivity: Some individuals with pollen allergies might experience oral allergy syndrome, where certain fresh fruits and vegetables can trigger mild allergic reactions due to cross-reactivity between pollen and certain proteins in these foods.
- Multiple Food Allergies: Some individuals are allergic to more than one type of food. Managing multiple allergies can be challenging and requires careful attention to ingredients.
It’s important to note that food allergies can range from mild to severe, and even a small amount of allergenic food can trigger a reaction in sensitive individuals. Anaphylaxis is a severe, potentially life-threatening reaction that requires immediate medical attention.
Precautions:
Managing food allergies requires a combination of caution, awareness, and preparedness. Here are some precautions to consider if you or someone you know has a food allergy:
- Know Your Allergens: Understand which specific foods trigger allergic reactions. Common allergens include peanuts, tree nuts, milk, eggs, soy, wheat, fish, and shellfish.
- Read Labels Carefully: Always read ingredient labels on packaged foods. Manufacturers are required to list significant allergens on their labels. Be aware of possible cross-contamination risks due to shared facilities or equipment.
- Avoid Cross-Contamination: Cross-contamination occurs when allergenic foods come into contact with non-allergenic foods. Use separate cutting boards, utensils, and cookware for preparing allergenic foods. Thoroughly wash hands and surfaces after handling allergens.
- Inform Restaurants and Servers: When dining out, inform the restaurant staff about your food allergies. Ask questions about ingredients and preparation methods. Choose restaurants with allergen-aware protocols if possible.
- Carry Medications: Always carry prescribed medications like epinephrine (EpiPen) if you have been prescribed one. Learn how to use it and ensure it’s not expired.
- Have an Action Plan: Develop an anaphylaxis action plan with your healthcare provider. This plan should outline the steps to take in case of an allergic reaction, including when and how to use epinephrine.
- Educate Family and Friends: Make sure close friends, family members, coworkers, and others you spend time with are aware of your food allergies and know how to respond in case of an emergency.
- Teach Children about Allergies: If your child has a food allergy, teach them about their allergens, what to avoid, and how to communicate their allergies to others.
- Pack Safe Snacks: When traveling or attending events, bring safe snacks and foods that you know won’t trigger an allergic reaction.
- Stay Informed: Food ingredients and manufacturing processes can change. Stay updated on food allergen information and be cautious about trying new foods without verifying their ingredients first.
- Be Wary of Hidden Ingredients: Some foods may contain allergens in unexpected ways. For instance, sauces, dressings, and gravies might contain allergenic ingredients.
- Check Cosmetics and Medications: Certain cosmetics and medications might contain allergenic ingredients. Check their labels for potential allergens before use.
- Collaborate with Healthcare Providers: Regularly consult with allergists or immunologists to discuss your allergies, receive updates on treatments or medications, and address any concerns.
Remember, individual circumstances may vary, so it’s essential to work closely with healthcare professionals to tailor your allergy management approach to your specific needs.
What are the food allergy blood tests?
Food allergy blood tests, also known as allergen-specific IgE tests or serologic tests, are diagnostic tools used to identify allergies to specific foods. These tests measure the levels of Immunoglobulin E (IgE) antibodies in the blood in response to specific food allergens. IgE antibodies are produced by the immune system when it encounters an allergen, and they play a role in triggering allergic reactions. There are a few different types of food allergy blood tests:
- ImmunoCAP (RAST) Test: This is one of the most commonly used blood tests for detecting food allergies. It measures the levels of specific IgE antibodies in response to various allergens, including food allergens. It’s a quantitative test that provides a numerical value indicating the concentration of IgE antibodies to each allergen.
- Multi-Allergen Screen Test: This test involves testing for a panel of common food allergens simultaneously. It can provide a quick overview of potential allergies, but it might not be as specific as individual tests for each allergen.
- Component-Resolved Diagnostics (CRD): This is a more advanced type of blood test that can provide additional information about the specific proteins within an allergenic food that triggers the immune response. It can help differentiate between true allergies and cross-reactivity.
- Food-Specific IgG Testing: Unlike IgE antibodies, IgG antibodies are not typically associated with immediate allergic reactions. Some alternative medicine practitioners offer IgG testing as a way to identify food sensitivities, but this approach is not widely accepted within the medical community as a reliable method for diagnosing allergies.
It’s important to note that while these blood tests can be helpful, they are not always definitive in diagnosing food allergies. The results should be interpreted by a qualified healthcare professional in conjunction with a thorough medical history and possibly other diagnostic tests, such as skin prick tests or oral food challenges. In some cases, false positives or false negatives can occur, so the clinical context and the patient’s symptoms are crucial for an accurate diagnosis. If you suspect you have a food allergy, it’s best to consult with a healthcare provider who specializes in allergies and immunology.
Treatment of Food Allergy:
The treatment of food allergies typically involves a combination of strategies to manage allergic reactions and prevent exposure to allergens. It’s important to note that there is no cure for food allergies, but various approaches can help individuals with food allergies live safely and comfortably. Here are some key aspects of the treatment of food allergies:
- Avoidance of Allergens: The primary approach to managing food allergies is to completely avoid the allergen(s) that trigger the allergic reaction. This involves reading food labels carefully, being aware of cross-contamination risks, and avoiding foods that might contain the allergen(s). For example, if someone is allergic to peanuts, they should avoid not only peanuts but also any products that contain or may have come into contact with peanuts.
- Education and Awareness: Individuals with food allergies should be educated about the allergens they are allergic to, how to read food labels, and how to identify potential sources of allergen exposure. This knowledge is crucial for preventing accidental consumption.
- Emergency Plan: People with severe allergies should have an emergency action plan in place. This plan may include steps to take in case of accidental exposure to the allergen, such as the administration of an epinephrine auto-injector (EpiPen). They should also inform family members, friends, and caregivers about the allergy and how to use the auto-injector if needed.
- Medical Management: Antihistamines may help relieve mild allergic reactions, such as hives or itching. However, for severe reactions like anaphylaxis, immediate administration of epinephrine is essential. Epinephrine helps to reverse the symptoms of anaphylaxis and can be life-saving. After using an epinephrine auto-injector, seeking immediate medical attention is crucial.
- Allergist or Immunologist Consultation: People with food allergies should consult with a board-certified allergist or immunologist. These specialists can perform allergy testing, guide managing allergies, and develop a personalized management plan.
- Oral Immunotherapy (OIT): This is a specialized treatment under the guidance of an allergist, in which the allergic individual is gradually exposed to increasing amounts of the allergen over time. The goal is to build a tolerance to the allergen, reducing the severity of allergic reactions. OIT is not suitable for everyone and should only be done under medical supervision.
- Research and Clinical Trials: Researchers are actively investigating new treatments for food allergies, including allergen-specific immunotherapy and biologics. Participating in clinical trials may provide access to experimental treatments and contribute to the advancement of allergy treatment options.
It’s important to work closely with healthcare professionals, particularly allergists or immunologists, to develop a comprehensive plan for managing food allergies. Treatment approaches can vary depending on the specific allergen, the severity of the allergy, and individual medical history. Always consult a medical professional for personalized advice and recommendations.

There are some interesting closing dates on this article however I don抰 know if I see all of them middle to heart. There is some validity but I will take maintain opinion till I look into it further. Good article , thanks and we wish more! Added to FeedBurner as nicely
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You definitely know what youre talking about, why throw away your intelligence on just posting videos to your site when you could be giving us something informative to read?
[…] Gluten Sensitivity Diagnosis: If celiac disease and wheat allergy are ruled out, and you continue to experience […]